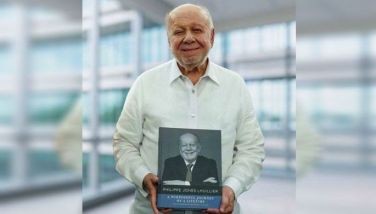
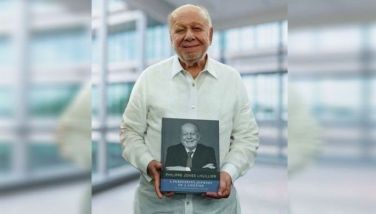
Just like ice cream man Paco Magsaysay, you, too can survive!

When artisan sorbetero Paco Magsaysay of Carmen’s Best was diagnosed with the earliest stages of chronic lymphocytic leukemia (CLL) in 2013, he decided to get a second opinion at the renowned MD Anderson Cancer Center.
Given its groundbreaking research, innovative clinical care, and technology, Paco was presented with a more hopeful prognosis.
When it comes to life-threatening diseases like cancer, early screening and diagnosis give patients and doctors a strategic ally in fighting the illness.
“Prior to my diagnosis, I would regularly get my annual executive checkup around my birth month, which is February,” shares Paco. “But that year, it got postponed multiple times.”
In January of the same year, Paco took an ice cream course in the US. He had to return a month later because his dad, Jun Magsaysay, was running for the Senate.
“So I didn’t get my executive checkup until after the elections in May,” relates Paco. “And that was when my doctor told me that my white blood count was a little bit off.”
Paco had to redo the blood test.
“And it was then that Dr. Joven Cuanang sat me down,” he shares. “If you know Dr. Cuanang, he jokes a lot.”
So Paco knew that something was definitely wrong with him just by looking at the amiable doctor.
“When he told me that I had leukemia, it felt like I was hit by a ton of bricks. It was a total shock because I wasn’t feeling anything,” he adds.
And that’s the problem with most cancers. You don’t feel anything, but the cancer cells are actually there — wreaking havoc in your body.
“That’s why getting an annual executive checkup is very important,” Paco advises.
In one of his early interviews, Paco said that in a way, “cancer was a blessing.”
“The disease was found and treated quickly. I had access to the best medical care. And the danger causes you to take inventory of your life and make time for what is more precious,” he shares.
Sadly, not everyone has access to the best cancer screening test, medical care and intervention like Paco.

The high cost of misdiagnosis
Finding out that you have cancer can be quite overwhelming. Disbelief is common. Other emotions soon follow. Hearing that you’ve been misdiagnosed, though, can be worse.
A diagnosis error can be defined as a diagnosis that is missed, wrong or delayed, as detected by some subsequent definitive test or finding. The ensuing harm results from the delay or failure to treat a condition present when the working diagnosis was wrong or unknown, or from treatment provided for a condition not actually present.
Despite medical technology advancements, diagnosing cancer often revolves around a doctor looking at slides under a microscope.
Accordingly, a pathologist may make a mistake in his or her analysis due to inexperience, stress, or haste.
Moreover, a pathologist usually does not have important information about the patient’s clinical picture, including his or her symptoms, medical history, or risk factors.
“If the doctor gives you the wrong treatment plan, it can do you more harm than good,” Paco adds.
Indeed, screening and tests are very important because most of the time, cancer doesn’t exhibit the signs and symptoms we are expecting.
And having a healthy lifestyle and healthy diet like Paco, who’s into basketball, can’t guarantee that you’ll be cancer-free.
Screening and diagnosis
If you have a risk factor, the doctor will advise you to get screened even if you’re not exhibiting any signs or symptoms yet.
“Diagnosis is the identification of the nature of an illness by examination of the symptoms,” explains Dr. Arnold Uson, president of the Philippine Society of Medical Oncology. “That’s the time when the patient already has bukol, or is already losing weight.”
According to Dr. Uson, both procedures should be done initially and immediately.
“If you have any symptoms, get yourself tested right away.”
Cancer-screening tests are designed to find cancers in their earliest stages, when the disease is most treatable.
Many cancer-screening tests have been found to lower the death rate from particular cancers.
According to the World Health Organization, early diagnosis improves cancer outcomes by providing care at the earliest possible stage, and is an important public health strategy in all settings.
Breast cancer is sometimes found after symptoms appear, but many women with breast cancer have no symptoms. This is why regular breast cancer screening is so important. Breast cancer image testing includes mammograms, breast ultrasound, and breast MRI. Oncologists could suggest a biopsy. This is done when mammograms, other imaging tests, or a physical exam shows a breast change that may be cancer.
Meanwhile, some lung cancers can be found by screening, but most lung cancers are found because they are causing problems. The actual diagnosis of lung cancer is made by looking at a sample of lung cells in the lab. A chest x-ray is one of the first screening procedures available. If the results of your history and physical exam suggest you might have lung cancer, more tests will be done. These could include imaging tests and/or biopsies of the lung.
A breakthrough screening test called biomarker testing provides a targeted treatment approach for cancer patients. Biomarker testing (also called tumor testing, tumor profiling, or tumor genetic testing) finds changes in your cancer that could help you and your doctor choose your cancer treatment.

Hope from within
In preparation for Lung Cancer Month this November, Hope from Within, a multi-stakeholder cancer advocacy campaign spearheaded by MSD in the Philippines, spotlights the importance of testing and diagnosis in an episode of its cancer conversation series dubbed “Tita Hope Talks: Winning vs. Cancer through Accessible Testing & Diagnostics.”
The discussion highlights why accessible testing and diagnostics is vital to improve the outcomes of cancer patients. Hosted by broadcast journalist and health advocate Niña Corpuz, Hope From Within sought to remind patients to be proactive in their health by consulting with their doctors, and at the same time encourage government leaders and decision makers to ensure that policies and programs on accessible cancer care are implemented properly.
Aside from Paco and Dr. Uson, the other resource speakers were Dr. Razel Nikka M. Hao, director IV of the Department of Health Public Health Services Team - Disease Prevention and Control Bureau; and Melissa Ongsue-Lee, VP for sales and marketing of Hi-Precision Diagnostics.
Access to better cancer care
Signed into law in February 2019, RA 11215, otherwise known as the National Integrated Cancer Control Act (NICCA), seeks to provide resources targeted toward cancer prevention, control, and awareness.
The NICCA also seeks to widen the scope of PhilHealth’s benefits packages to primary care screening, diagnosis, and end-of-life care for all stages and types of cancers, for both children and adults.
Another development in cancer care: the Department of Budget and Management (DBM) recently announced that the national government’s P529.2 million Cancer Assistance Fund may still be used until Dec. 31 of this year.
This came following the DBM and the Department of Health’s (DOH) release of a joint memorandum circular (JMC) prescribing the Implementing Guidelines for the fund.
The CAF is a mechanism under Republic Act No. 11215 or the National Integrated Cancer Control Act, which seeks to provide integrated and holistic support for cancer treatment and management.
It aims to complement and supplement existing financial support mechanisms exclusive for cancer patients, persons living with cancer, and cancer survivors.
Pursuant to the circular, the CAF will also fund outpatient and inpatient cancer control services, including but not limited to diagnostics, therapeutic procedures, and other cancer medicines needed for the treatment and management of cancer and its care-related components.
* * *
To learn more about Hope From Within’s cancer advocacy programs, visit https://hopefromwithin.org/ or follow their Facebook page https://www.facebook.com/Hopefromwithinph/.